Patent Ductus Arteriosus
________________________________________________________________________
KEY POINTS
- Patent ductus arteriosus (PDA) is a birth defect that causes abnormal blood flow in the heart.
- Your baby may not need treatment, or your baby may need medicine or surgery to close the PDA.
- Follow your child’s healthcare provider's instructions. Ask your provider if there are activities your child should avoid and when your child can return to normal activities.
________________________________________________________________________
What is patent ductus arteriosus?
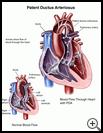
Patent ductus arteriosus (PDA) is a birth defect that causes abnormal blood flow in the heart.
Before birth, a baby’s blood does not need to go through the lungs to pick up oxygen because the baby gets oxygen-rich blood from the mother. A blood vessel called the ductus arteriosus lets blood go around the baby’s lungs before birth. At birth, when the baby’s lungs fill with air, this blood vessel is no longer needed, and normally it closes soon after birth. When it does not close, it is called a patent ductus arteriosus, or PDA. In a child with PDA, some of the blood that should go to the rest of the body through the aorta goes back to the lungs instead.
What is the cause?
The exact cause of this birth defect is not known.
This problem is common in premature infants, especially if their lungs are not mature. It is rare in full-term babies. Other risks for PDA include:
- Genetic problems such as Down syndrome. Genes are inside each cell of the body and are passed from parents to children. They contain the information that tells the body how to develop and work.
- Mothers who had rubella during pregnancy
- Having other heart defects
- Having siblings who were born with PDA
What are the symptoms?
Babies who have a small opening often have no symptoms, but PDA causes a whooshing sound, called a murmur, as blood moves through the heart. Healthcare providers can hear the murmur with a stethoscope.
If the PDA is large, a baby may not gain weight easily. The baby may get short of breath and sweat when crying or playing. An older child with PDA may not be able to exercise as much as normal and may have lung infections often. A PDA can also increase the risk of an infection in the heart called endocarditis.
How is it diagnosed?
Your healthcare provider will ask about your child's symptoms and medical history and examine your child.
Tests may include:
- An echocardiogram, which uses sound waves (ultrasound) to show pictures of the heart and how well blood is flowing through it
- Chest X-ray
- An ECG (also called an EKG or electrocardiogram), which measures and records your child’s heartbeat
How is it treated?
A PDA may close by itself and not need treatment. In premature babies, medicine can be used to help the PDA close.
If the PDA is large or does not close by itself, your baby will need surgery. Your baby may need to take medicines until strong enough to have surgery. Two types of surgery may be done to close the defect:
- Heart catheterization uses a small tube called a catheter inserted into a blood vessel. Your baby’s healthcare provider will use tools put through the catheter to repair the defect by plugging the opening with a small plastic device.
- Surgery to close the defect may be needed.
How can I take care of my child?
Follow your child’s healthcare provider's instructions. Ask your provider:
- How and when you will get your child’s test results
- How long it will take for your child to recover
- If there are activities your child should avoid and when your child can return to normal activities
- How to take care of your child at home
- If your child should take antibiotic medicine to prevent infection before having dental work or procedures that involve the rectum, bladder, or vagina
- What symptoms or problems you should watch for and what to do if your child has them
Make sure you know when your child should come back for a checkup. Keep all appointments for provider visits or tests.
Last modified: 2022-01-03
Last reviewed: 2018-11-26